Yes! ACDIS awards CCDS/CCDS-O CEUs to authors published in two of our publications.
First, contributors can submit articles for publication in the CDI Journal, ACDIS’ bimonthly members-only publication. Contributors published in the Journal receive 0.5 CEUs per 350 published words and articles tend to be around the 750-1,500 word mark. Each Journal edition is centered on a theme and contributors are welcome to use that theme as a jumping off point for their articles, but we always like to include some clinical and coding topics as well. All the topics and deadlines are posted in our Publications FAQ section.
Secondly, ACDIS CDI Leadership Council members can submit articles for publication in the CDI Leadership Insider (CLI), the Council-specific publication that goes out the second Monday of the month. The articles in the CLI tend to be 750-1,000 words long and contributors receive 0.5 CEUs per 350 published words. The topics are chosen by the contributor, though if contributors would like help, they can email Associate Editorial Director, Publications & Membership, Linnea Archibald (larchibald@acdis.org) for assistance. The remaining 2022 Council term deadlines are as follows:
- April 11, 2022 edition
- Deadline: March 28, 2022
- May 9, 2022 edition
- Deadline: April 25, 2022
- June 13, 2022 edition
- Deadline: May 30, 2022
- July 11, 2022 edition
- Deadline: June 27, 2022
- August 8, 2022 edition
- Deadline: July 25, 2022
And finally, while ACDIS accepts contributor articles for the ACDIS Blog and CDI Strategies, they are not awarded CEUs. These articles tend to be a bit shorter and less formal, running about 500-700 words. Articles submitted for publication on the Blog or in CDI Strategies are reviewed on a rolling basis and offer new authors a “training ground” in a less formal setting.
Our testing partner, Prometric, owns and operates a network of more than 14,000 global testing centers. You can find COVID-19 related information on the Prometric website under the COVID-19 Update tab.
Prometric also supports remote proctoring, allowing candidates to take their exams from their own homes or elsewhere meaning candidates are still able to take the CCDS/CCDS-O exam in light of COVID-19.
If you have further questions, please contact our Customer Care at customerservice@hcpro.com or 800-650-6787.
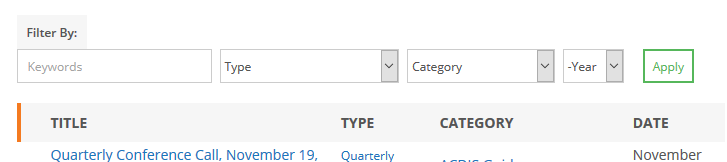
The Resource Library has search and filter options to help you narrow your search. To ensure you’re finding all potential matches to your search, we suggest that you search for a single word in the “Keywords” box (e.g., “sepsis” rather than “sepsis validation”). You can also filter by resource type using the dropdown menu, by topic category, and by publication year.
Yes, but please include attribution to ACDIS and the original author as follows:
- ACDIS. Last name, first name. Name of organization, Publication date. Website link.
While the majority of the resources in the Resource Library are only available to ACDIS members, there are quite a few places non-members can access free educational tools. You’ll find unlocked resources in the following sections:
- Free & Sponsored Resources: From time to time, ACDIS’ sponsors provide members with valuable insight into CDI topics of the day. These free webinars and focused research briefs can all be found in this section. Additionally, you’ll find free ACDIS webinars here too.
- Videos: If you’re looking for guidance on the ACDIS website offerings, tutorials, and recordings of the Chapter Advisory Board calls, look in this section of the website.
- The ACDIS Podcast: The podcast is a free biweekly show focused on the latest news and tips in the CDI industry. Each episode is hosted by ACDIS Director Brian Murphy and one of our expert Boot Camp instructors and features an industry guest. You can register and tune in for the live show every other Wednesday at 11:30 a.m. eastern, or Subscribe on Apple Podcasts, Google Play, or Spotify and listen on the go. The on-demand podcast goes live the Friday following the live show date.
- Position papers: These papers are the association’s official, consensus stance on an issue. ACDIS position papers set a recommended standard for the CDI industry to follow. They advocate on behalf of a certain position or offer concrete solutions for a particular problem. All current members of the ACDIS Advisory Board must review/approve a position paper and are encouraged to materially contribute to its creation.
If you’re looking for free CDI articles, items published in ACDIS’ weekly eNewsletter, CDI Strategies, and on the ACDIS Blog are all available to both members and non-members alike.
Sample educational tools, job descriptions, policies and procedures, and query forms found in the Resource Library are contributed by the ACDIS membership and reviewed for compliance, helpfulness, and accuracy by the ACDIS Forms & Tools Library Committee on a rolling basis.
If you have a tool, sample, or resource to share, please send it to ACDIS Associate Editor Jess Fluegel (jfluegel@acdis.org).
Sample educational tools, job descriptions, policies and procedures, and query forms found in the Resource Library are contributed by the ACDIS membership and reviewed for compliance, helpfulness, and accuracy by the ACDIS Forms & Tools Library Committee on a rolling basis.
The Forms & Tools Committee is comprised of 8-10 CDI professionals from varying professional backgrounds, organization types, and job title, along with a committee coordinator from the ACDIS leadership team. They meet monthly to review all submitted materials and determine their worthiness to be published in the Library.
While the Committee does not edit submissions, they do pen recommendations to go along with each sample to help those adapting samples for their own use. While the samples aren’t a one-size-fits-all solution for all CDI programs everywhere, samples the Resource section of the website can be a starting point for developing your own forms, tools, policies, and procedures.
If you have a tool, sample, or resource to share, please send it to ACDIS Associate Editor Jess Fluegel (jfluegel@acdis.org).
ACDIS is a community that welcomes idea sharing, networking, creative problem solving, and free and open speech and debate. As a result, we publish many papers, articles, news briefs, and informal commentary across our website. The question some members ask is: What articles represent ACDIS’ official stance, guidance, or advice on a particular question or issue?
To answer this question, we have established a “Hierarchy of Authority” detailing which articles are considered official ACDIS advice or guidance, and which are not. The most authoritative “ACDIS endorsed” publications are listed first.
1. ACDIS position papers: ACDIS position papers are the association’s official, consensus stance on an issue. ACDIS position papers set a recommended standard for the CDI industry to follow. They advocate on behalf of a certain position or offer concrete solutions for a particular problem. All current members of the ACDIS Advisory Board must review/approve a position paper and are encouraged to materially contribute to its creation. You can find ACDIS position papers here: https://acdis.org/resources?type=12
2. ACDIS white papers: White papers are next in the ACDIS hierarchy of authority. An ACDIS white paper discusses CDI best practice, advances new ideas, increases knowledge, or offers suggestions for administrative simplification. These can be written by a single ACDIS Advisory Board member, a smaller subset of the board, or can be written by external sources (when they are, they are clearly labelled as such). White papers are less formal than a position paper but are peer-reviewed. You can find ACDIS white papers here: https://acdis.org/resources?type=14
3. CDI Journal: Articles in our bi-monthly members-only CDI Journal are subject to editorial review and extensive editing prior to publication. But unless otherwise noted they do not represent official ACDIS recommendation or policy. ACDIS’ CDI Journal strives to use a variety of sources in its articles to ensure fair and accurate coverage. Occasionally the CDI Journal publishes opinion pieces and columns from industry experts. We strive to clearly mark these as such, and advice provided is general in nature and CDI staff should review the information to ensure compliance. While ACDIS Advisory Board members frequently write articles for CDI Journal the opinions expressed represent their own, not those of the association. You can find current and archived issues of CDI Journal here: https://acdis.org/articles/archive?publication=1
4. CDI Strategies: Unless otherwise noted CDI Strategies articles are summations of relevant news articles, recaps of local chapter activity, notifications of articles or downloads to the ACDIS website, or Q&As with industry representatives. These are curated, edited, and uploaded by ACDIS editorial staff but not peer-reviewed. You can find an archive of CDI Strategies articles here: https://acdis.org/articles/archive?publication=2
5. Forum posts, comments, social media, and the ACDIS Blog: Posts in ACDIS Forum, comments appended to the end of articles or on ACDIS Blog, and posts or replies to ACDIS social media platforms including Facebook, Instagram, and Twitter, are automatically assumed to be the opinions of the person posting the comment. Inappropriate or offensive posts will be removed.
To sum up, unless an article is a position paper, or an ACDIS white paper (i.e., a white paper written or approved by the ACDIS advisory board, not from an outside source), it is not considered official ACDIS guidance.
General note regarding articles on this website
Please note that ACDIS is an association of professionals governed by an elected advisory board and administrators. It is not a regulatory body. As in all matters, please refer to your manager, compliance department, and/or legal counsel before implementing changes or altering your organization’s policies and procedures.
Does ACDIS Radio offer CEUs for listeners or materials or other handouts?
No, ACDIS Radio does not meet requirements for offering CEUs--at 30 minutes it is not long enough, and it does not have learning objectives, occasionally promotes products, and is conversational and not formal in nature. ACDIS Radio also does not provide materials to listeners in advance. From time to time guests will share .ppts or other materials and these are posted in the ACDIS Radio archives with the recording of the show once it is completed.
How is the examination administered?
To become a Certified Clinical Documentation Specialist (CCDS), a candidate must pass the examination. It is offered by computer at more than 200 AMP Assessment Centers located around the country (click on your state for locations and directions).
Candidates who apply to take the examination will be contacted when they have been approved to take the examination.
Candidates have four months/120 days from the date their name is submitted to AMP, the examination testing company, to schedule and take their examination.
There are no application deadlines (except for the examination given at the conference) and a candidate who meets eligibility requirements may submit an application and fee at any time. The fee will not be processed until the application is approved.
What are the eligibility requirements?
Candidates for the CCDS designation must meet educational and work experience requirements.
The candidate for the Certified Clinical Documentation Specialist (CCDS) exam will meet one of the following three education and experience standards and currently be employed as either a concurrent or retrospective Clinical Documentation Specialist:
- An RN, RHIA, RHIT, MD, or DO and two (2) years of experience as a concurrent/retrospective documentation specialist in an inpatient acute care facility using the United States IPPS system.
- An Associate’s degree (or equivalent) in an allied health field (other than what is listed above) and three (3) years of experience as a concurrent/retrospective documentation specialist in an inpatient acute care facility using the United States IPPS system. The education component must include completed college-level course work in medical terminology and human anatomy and physiology.
- Formal education (accredited college-level course work) in medical terminology, human anatomy and physiology, and disease process, or the AHIMA CCS credential, and a minimum of three (3) years of experience in the role as a concurrent/retrospective documentation specialist in an inpatient acute care facility using the United States IPPS system.
*Years of experience is defined as full time employment or greater than 2,000 hours/year
What is a concurrent documentation specialist?
The concurrent documentation specialist:
- Reviews medical records daily and in the current time, while the patient is hospitalized
- Works collaboratively using real-time conversation with physicians and medical team members caring for the patient
- Uses his or her clinical knowledge to evaluate how the medical record will translate into coded data, including reviewing provider and other clinical documentation, lab results, diagnostic information, and treatment plans
- Communicates with providers, whether in verbal discussion or by query, for missing, unclear, or conflicting documentation
- Educates providers about optimal documentation, identification of disease processes that reflect severity of illness, complexity, and acuity to facilitate accurate coding
- Understands complications, comorbidities, severity of illness, risk of mortality, case mix, and the impact of procedures on the billed record, and shares this knowledge with providers and members of the healthcare team
What is a retrospective documentation specialist?
The retrospective documentation specialist:
- Daily reviews medical records of post discharge, pre-bill records
- Works collaboratively using real-time conversation with physicians and medical team members who cared for the patient
- Uses his or her clinical knowledge to evaluate how the medical record will translate into coded data, including reviewing provider and other clinical documentation, lab results, diagnostic information, and treatment plans
- Communicates with providers, whether in verbal discussion or by query, for missing, unclear, or conflicting documentation
- Educates providers about optimal documentation, identification of disease processes that reflect severity of illness, complexity, and acuity to facilitate accurate coding
- Understands complications, comorbidities, severity of illness, risk of mortality, case mix, and the impact of procedures on the billed record, and shares this knowledge with providers and members of the healthcare team
Equivalent foreign medical graduate experience documenting in a medical record as a clinician or resident does not meet the experience requirement.
